Concussion Protocol 101 guide
What to do with potential concussions in your organization
WHAT IS A CONCUSSION PROTOCOL?
- Concussion protocol is an agreed upon plan for managing concussions.
- Anyone who handles concussions needs to have a concussion protocol in place.
- Concussion protocol documents all processes from pre-activity education to clearance policies.
- Effective concussion protocol takes into consideration that every concussion is different.
- Successful concussion protocol has a variety of assessment tools and involves multidisciplinary team members.
- Concussion protocol needs to be reviewed and updated with best practices annually
1. CONCUSSION PROTOCOL BASICS
WHAT IS A CONCUSSION PROTOCOL/POLICY?
A concussion protocol is an organization’s set of policies, tools, and assessments for caring for a concussion. It outlines how the concussion care team prepares for and responds to this injury. You may think a “concussion protocol” implies a strict, written policy that instructs healthcare providers to treat every patient and every concussion the same. However, trained healthcare providers know that a concussion requires an individualized care approach. For the purposes of this article, “protocol” and “policy” mean the same thing.
A concussion protocol (policy) is used to ensure everyone involved knows what to do when a concussion happens.

WHO NEEDS A CONCUSSION PROTOCOL?
An organization needs a concussion protocol when they have children or adults who may be at risk for a concussion. Keep in mind: concussions don’t just happen in sports. They can happen at work, in auto accidents, or from falls. They happen to young children, adolescents, and adults. Learn more about concussions beyond athletics.
Most states in the United States have laws requiring schools to have protocols for their athletes. Ontario, Canada has also passed legislation requiring removal from sport and return to activity protocols for youth athletes. These laws are a step in the right direction to ensuring proper care after a concussion. However, there are still many countries and communities that lack written concussion protocols.
The person responsible for creating a concussion protocol depends entirely on the individual setting. In general, a healthcare provider familiar with concussions should be the one to create the protocol.

WHAT STAKEHOLDERS ARE INVOLVED IN FOLLOWING A CONCUSSION PROTOCOL?
The best concussion protocols involve a variety of teammates and care stakeholders. At a minimum, a concussion protocol should involve at least these individuals:
- Point Person: This is the person who will be in charge of the concussion care team. They may be involved in both diagnosis and management. They’ll manage referrals and provide return to activity clearance. Ideally, this person would be a Credentialed ImPACT Consultant (CIC) – a qualified healthcare provider who has been specially trained in the management of a concussion.
- Athletic Trainer: They will likely conduct a sideline evaluation for student athletes. They also coordinate care at the school for students. They are involved in progressive return to activity. Learn more about the AT's role in concussion care in this comprehensive e-guide.
- Chiropractor: Chiropractors may be on the sideline of sports games and practices to triage, make removal from activity decisions, and refer for further assessment. Learn more about the chiropractor’s role in concussion care in this comprehensive e-guide.
- School Nurse/Counselor (for school settings): The school nurse is someone who can help monitor students’ symptoms. They work with school staff to make sure academic adjustments are implemented as the student returns to school after a concussion.
- Teachers (for school settings): Teachers can also monitor signs and symptoms after a concussion. They can coordinate with athletic trainers and school nurses to make sure students get the right academic adjustments after a concussion.
- Rehabilitation professionals: Physical therapists, occupational therapists, speech language pathologists, and others. They help target rehab for specific areas that are affected after a concussion. Learn more about the physical therapist's role in concussion care and rehab in this comprehensive e-guide.
- Parents: it’s important to identify the role of parents in symptom monitoring. They also can ensure daily regulation and healthy habits for their children.
Once you have your concussion care team assembled, make sure they have the training they need. Use our library of training courses to ensure everyone is on the same page when it comes to concussion care.
ARE THERE STANDARD CONCUSSION PROTOCOL STEPS I CAN FOLLOW
While concussion protocols differ by setting, most healthcare providers agree on the key concussion protocol steps that should be included. Concussion protocol requirements can also differ depending on country, state, or local laws.
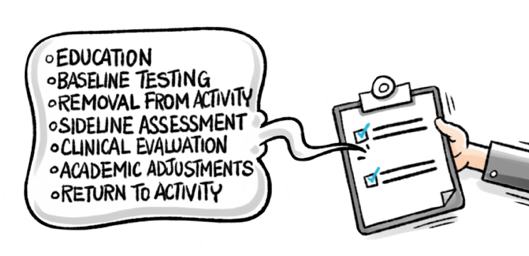
At a minimum, concussion protocol steps should include:
- Concussion definition
- Concussion education including signs, symptoms, and immediate recognition. (Use this removal from activity guide to educate stakeholders on the importance of reporting concussion symptoms.)
- Pre-season baseline testing (Want students to take their ImPACT Baseline Test from home? Distribute unique testing links in the Customer Center or have them purchase their own baseline test online.)
- Removal from activity criteria
- Sideline assessment procedures
- Clinical evaluation procedures
- Academic adjustment guidelines
- Return to activity procedures and guidelines (Use this return to activity checklist to make sure you've covered all the bases)
With all these key elements, you’ll have a great start to a concussion management protocol.
2. HOW TO CHECK FOR CONCUSSION

WHAT DOES A SIDELINE EVALUATION ENTAIL?
Sideline evaluations are a critical early measure in checking for a concussion and determining next steps in the concussion care process. After a bump, blow, or jolt to the head, a healthcare provider trained to recognize concussions should follow a well-defined sideline process.
Athletic trainers are frequently the first responders in the case of an athletic head injury. Learn about their important role.
Because a concussion often happens without an athlete losing consciousness, a healthcare provider must use screening for head injury in other ways. Without a full sideline assessment, student athletes may return to play prematurely and be at risk for negative consequences. The brain can swell and cause lasting damage or increased long-term symptoms.
A sideline evaluation should include a symptom check and memory screening, cognitive functioning, and concentration. Its purpose is to determine if a trip to an emergency department is necessary. If not, they’ll determine if removal from participation with continued monitoring is warranted.
Brief tests like ImPACT Quick Test can help a healthcare provider quickly check cognitive function. Sideline professionals should also be on the lookout for worsening symptoms.

WHAT IS CONCUSSION SCREENING?
A concussion screening is a brief evaluation conducted by a trained healthcare provider. Its purpose is to determine the presence of a concussion after a blow to the head.
A trained healthcare provider will document whether or not there was a hit to the head and the location of impact. They will check for visible injury to the head or body. They’ll record if there was loss of consciousness, amnesia before or after the event, and any early concussion signs.
They will ask the patient about any symptoms they feel. They’ll likely conduct a brief cognitive screening to help make the removal from activity decision. They will determine if the patient requires an emergency department visit. The healthcare provider will continue monitoring for any new symptoms that might appear after the injury.

WHAT IS BASELINE COGNITIVE TESTING?
A baseline test measures your brain function in a healthy state. If you have an injury, healthcare providers can use a post-injury test to help determine if you have a concussion. It measures reaction time, memory capacity, speed of mental processing, and executive functioning of the brain. Baseline testing is recommended to be completed annually to ensure an up-to-date record of a patient’s normal functioning.
A trained healthcare provider can compare a post-injury test to a patient’s baseline. This way, they’ll have an objective idea of the extent of the injury. While concussions aren’t preventable, baseline testing is a great way to ensure someone is prepared if a concussion ever happens.
If you don't have time or resources to group baseline test all your test takers, you have two other time-saving options:
- Send test takers a unique baseline testing link via email from your Customer Center. The tests come out of your normal testing bank.
- Have test takers pay for a baseline test individually and take it at home.

WHAT IS POST-INJURY TESTING?
It measures the same areas as baseline testing. Healthcare providers use post-injury testing to understand a patient’s cognitive functioning after a jolt to the head. A post-injury clinical report is compared to a patient's baseline to show deficits in cognitive functioning and reaction time.
Post-injury testing can still be used if a test taker doesn’t have a baseline. This is thanks to normative data, which provides average scores within an age range. Post-injury testing is done by trained healthcare providers who use the test and other data to help evaluate a concussion. They’ll use it to develop an appropriate treatment plan to provide the most efficient recovery pattern.
WHAT IS SANDBAGGING AND HOW DOES IT IMPACT CONCUSSION TESTING?
Sandbagging is when a test taker deliberately underperforms on a baseline concussion test. Many athletes are aware that their ability to return to activity is determined by their baseline results. They may perform poorly to lower the threshold of comparison when their healthcare provider is deciding whether or not to clear them. It is not easy to sandbag during baseline testing because of built in validity indicators that flag suspicious results.
Read more about sports concussions and sandbagging as well as the preventative measures you can take.
3. CONCUSSION SIGNS, SYMPTOMS, DIAGNOSIS AND TREATMENT

WHAT ARE THE SIGNS OF A CONCUSSION?
Concussion may have several signs visible to those familiar with an individual who’s recently experienced a blow to the head. Because a concussion is a functional injury rather than a structural one, they do not show up on CT scans or MRIs. There are many signs that can point towards a concussion.
Signs of a concussion can include:
- Loss of consciousness
- Change in behavior
- Sleeping much more or less than usual
- Grades dropping for a student
- Increased anxiety
- Repeated vomiting
- Dizziness
- Headaches
- Distractible
- Light or noise sensitivity
- Feeling worse in the afternoon compared to morning

HOW DO I EDUCATE STUDENT ATHLETES ON SYMPTOM REPORTING?
Educating student athletes on concussions can seem like an overwhelming process, but there are plenty of resources available to help. You can look through helpful concussion care resources to educate parents and student athletes on concussions.
You should provide concussion education to all stakeholders. This includes student athletes, coaches, parents, school staff, and sports officials. Education should take place prior to an athletic season, or at the beginning of each year for students.
These are key elements of a concussion education program:
- What a concussion is
- Signs and symptoms
- Why it’s so important to report a concussion, both for individual student athletes and teammates
- What baseline testing is and why it’s done
- Who to talk to if an athlete suspects a concussion
- What happens after a concussion - expectations for follow up care
Education can be delivered in a few ways, depending on your resources. If you’re working with athletes, a preseason meeting is a great place to provide education. You have the option of offering web-based education as well. At any rate, providing this concussion education information and being available to answer any questions is a good start. You can also direct parents and student athletes to this Concussion 101 Guide that meets state concussion education requirements.

WHO'S RESPONSIBLE FOR DIAGNOSING A CONCUSSION?
A healthcare provider trained in concussion care should always be the one to diagnose a concussion. Concussion diagnosis should not be done by coaches, parents, or student athletes. Healthcare providers have tools and assessments to help recognize concussions. They know the next steps to take if a concussion is suspected. Because concussions are hard to identify, it’s important that diagnosis is done by someone who’s trained to do so.
WHEN TO SEEK MEDICAL CARE FOR A SUSPECTED CONCUSSION?
If a concussion is suspected, it’s important to contact a trained healthcare provider immediately. It’s recommended that individuals with a concussion have a 1-2 day period of rest followed by progressive increases in activity. This return to activity should always be monitored by a trained healthcare provider.
Most providers will try to see their patients 24-72 hours after the injury to assess their functioning. Every concussion is different. This means that there isn’t a “one size fits all” approach to healing after a concussion. A trained concussion care provider can assess patients' individual symptoms and provide a treatment plan that helps them get better.

WHAT ARE RETURN TO LEARN AND RETURN TO PLAY PROTOCOL GUIDELINES?
Return to learn guidelines are the processes used to get a student back to full cognitive activity after a concussion. A concussion affects the way the brain functions. Students recovering from a concussion may have a difficult time adjusting to normal school activities.
Return to learn guidelines can include temporary academic adjustments or longer academic accommodations. In rare cases, formal academic modifications in the form of a 504 or Individualized Education Plans in the US may be required. In most cases, short-term informal academic adjustments may be all a student needs. These can include class breaks, early dismissal between classes, reducing computer screen exposure, extra time to take tests, and more.
Return to play guidelines are the gradual processes used to ensure an athlete’s safe return to activity after a concussion. Most healthcare providers recommend a 6-step approach to return to activity.
Return to activity steps include:
- Symptom-limited activity
- Light aerobic exercise
- Sport or activity specific exercise
- Non-contact training drills
- Full contact practice
- Return to sport
Use this return to activity checklist to make sure you've covered all the bases.
Every concussion is different, so every return to activity approach will be different. Healthcare providers will prescribe exercises specific to the activity the patient wants to return to. Return to activity exercises will help ensure a patient gets back to normal functioning.
Want an easy reference guide on setting up a concussion protocol? Download step-by-step instructions.