Chiropractor’s Role in
Concussion Management
Chiropractors may use ImPACT for patients ages 12-80 (ImPACT Pediatric for patients 5-11) to help determine the cause of some of the signs and symptoms the patient is experiencing, as well as use it to monitor progress throughout return to academics and sport. ImPACT consists of 8 neurocognitive test batteries that measure visual and verbal memory, reaction time, and processing speed. It also includes a 21 item concussion symptom scale that you may use to cater your exam and make sure you address any symptoms the patient is reporting. After administration, a detailed clinical report is automatically generated that you can use to help guide rehab plans.
ImPACT is a critical portion of the examination because it provides objective data that can be used to help guide treatment decisions. In instances where the patient doesn’t have an established baseline, the chiropractor can compare ImPACT post-injury test results to normative data. ImPACT can be administered remotely or in-person, so chiropractors don’t need to have large computer labs or additional resources to use ImPACT.
Download the Chiropractor's Role in Concussion Management
Download the complete Chiropractor's Role in Concussion Management to learn more about resources, tools, and methodologies a chiropractor may use for concussion assessment and management.
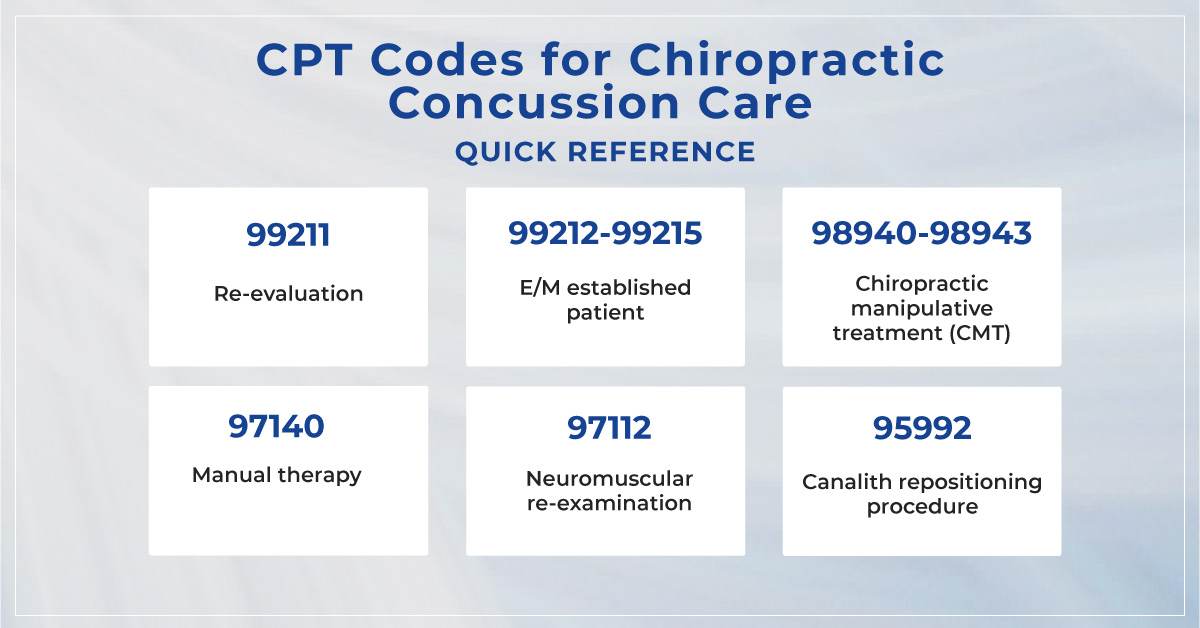
As a doctor of chiropractic, you may be able to get reimbursed for a variety of techniques and modalities used for examining concussion patients.
Commonly used ICD-10 codes for chiropractic concussion care:
Concussion
- S06.0X0 - Concussion without loss of consciousness (LOC)
- S06.0X0A - Initial encounter
- S06.0X0D - Subsequent encounter
- S06.0X0S - Sequela
- S06.0X1 - Concussion with LOC 30 minutes or less
- S06.0X1A - Initial encounter
- S06.0X1D - Subsequent encounter
- S06.0X1S - Sequela
- S06.0X9 - Concussion with LOC of unspecified duration
- S06.0X9A - Initial encounter
- S06.0X9D - Subsequent encounter
- S06.0X9S - Sequela
Based on a presentation given by Dr. Jordan Knowlton-Key, Doctor of Chiropractic, at the 2022 Concussion Care Virtual Conference.
This guide is based on the scope of doctors of chiropractic in the U.S. The extent to which chiropractors can be involved in concussion management differs by state. Always check your state’s scope of practice to confirm what roles and responsibilities you may have within the concussion care team.