Role of Athletic Trainers for Concussion Care
Based on a presentation given by Tamara McLeod, Professor and Director of Athletic Training at A.T. Still University, at the 2022 Concussion Care Virtual Conference.
Benefits of an Athletic Trainer
- Specialized Training - Athletic trainers receive specific training in concussion management.
- Education - Athletic trainers provide important concussion education to student-athletes, parents, coaches, and school staff.
- Standard of Care - Schools with athletic trainers are at least 4 times more likely to recognize and diagnose concussions than schools without them.
Athletic trainers are vital members of any concussion care team. They help maintain the health of not only athletes but also a variety of other patients. Learn more about their specific role and why an athletic trainer is important for your organization’s concussion protocol.

What Is an Athletic Trainer?
Athletic trainers are skilled healthcare professionals who work alongside physicians. Their specialized training and diverse skill set allow them to make removal from activity decisions, assist with injury prevention, and provide emergency and rehabilitative care.
Unlike personal trainers, athletic trainers are required to graduate from an accredited master’s program that supplies a curriculum and clinical training based on the medical model. They may also complete athletic training certifications and take annual continuing education courses to stay up to date on the best practices in concussion care.
What Does an Athletic Trainer Do?
Athletic trainers offer care to all types of patients and can work in a wide range of settings. (Learn about the athletic trainer's role in the physician practice setting.) This can include providing primary care, outpatient rehab support, and education for injury prevention. Specifically, at the school and youth sports levels, athletic trainers serve as a liaison between outside medical professionals, school administration, and parents.
They are instrumental in maintaining the safety of student-athletes and ensuring an organization’s concussion protocol is airtight. Athletic trainers do this by being the main point of contact for concussion care and in some cases, helping identify the policies, tools, assessments, and stakeholders to include. Having these procedures in place helps protect schools from potential lawsuits by documenting their concussion management plan and showing they are up to date on the best practices for treatment.
Here are a few other areas athletic trainers are responsible for:
- Educating athletes, parents, school staff, and coaches about concussion and injury prevention
- Developing emergency action plans
- Conducting examinations and assessments of injuries
- Making removal from activity decisions
- Coordinating rehabilitative care with athletes and parents
- Establishing a return to play protocol
- Suggesting academic adjustments for return to learn
For more information on how to protect your organization from lawsuits, read the Liability in Concussion Care 101 Guide.
Athletic Trainer Scope of Practice
Athletic trainers are educated and trained to work with the multidisciplinary team throughout the entire continuum of concussion care.
The BOC Practice Analysis provides 5 domains of athletic training practice each including elements that relate to concussion care.
Domain 1: Risk Reduction, Wellness, and Literacy - includes identification of risk factors which relates to pre-participation physical exams.
Domain 2: Assessment, Evaluation, and Diagnosis - covers concussion assessment and diagnosis.
Domain 3: Critical Incident Management - relates to on-field management and activation of the Emergency Action Plan (EAP) for potential injuries that may be worse than a concussion.
Domain 4: Therapeutic Intervention - covers concussion treatment and following up care.
Domain 5: Healthcare Administration and Professional Responsibility - covers elements of concussion policy, protocols, and standing orders.
The NCAA Athletics Healthcare Administration Best Practices suggests that in compliance with laws and practice acts, licensed medical providers, including athletic trainers, should have unchallengeable medical authority in decision-making regarding injuries, including concussion. It also states that it’s critical for athletic trainers to educate stakeholders on how athletic trainers are qualified to be involved in all aspects of concussion care.
Preseason preparation
The athletic trainer is critical in preseason preparation. This should include:
- Pre-participation exams (PPE)
- Emergency action plans (EAP)
- Policy review (statewide and locally)
- Educating stakeholders

Pre-participation exam
Pre-participation exams should ask about athletes’ concussion history. If they indicate that they have had a prior concussion, follow up with additional questions to get more information.
How many diagnosed concussions have you had?
When did the concussion(s) occur?
What symptoms did you experience?
What was the duration of those symptoms?
Do you have any diagnosed learning disabilities such as ADHD?
Do you regularly experience motion sensitivity?
Do you or someone in your family have a diagnosed mood disorder?
How long did it take you to recover from your previous concussion(s)?
How much time did you miss from sports / school / work / etc.?
Did you have any academic adjustments in place?
Were you referred for rehab?
Are you currently taking any medications?
Gathering more information is important because depending on their answers to these questions, they may be predisposed to a prolonged recovery and you may want to initiate academic adjustments and referrals earlier.
Emergency Action Plan (EAP)
Athletic trainers are trained to be involved with emergency action planning and are often the point people when the EAP is activated. EAPs should be venue-specific and rehearsed with involved personnel. Athletic trainers should know the location of the closest emergency department including the ambulance entrance. The EAP should include how you will document, especially from the on-field standpoint. The EAP should be reviewed and approved by school administration as well as legal / risk management to ensure that everyone is on board with the plan.
Concussion Policy and Protocols
Athletic trainers are in charge of reviewing and revising concussion protocols to stay compliant with local and state laws.
Baseline Testing
Athletic trainers are trained to be involved in concussion baseline testing. It should be a multimodal baseline that evaluates symptoms, cognition, motor control, and ocular motor function.
Sideline Evaluation
The athletic trainer plays a critical role in initiating the on-field exam, determining the need for emergency referral, and serial sideline assessments. They also educate patients and parents following a suspected concussion on what they did in their evaluation, what red flags to look out for, and recommendations for follow up care.

As part of the sideline exam, the athletic trainer would clear these on-field signs that would indicate an immediate diagnosis of at least a concussion:
- Loss of consciousness (LOC)
- Ataxia
- Tonic posturing
- Post-traumatic seizure
Once the on-field signs are cleared, more in-depth assessments can be done such as ImPACT Quick Test - a 5-minute sideline assessment tool. If a concussion is suspected, the athlete should be immediately removed from play and referred for further evaluation.
Follow-up assessments
The athletic trainer is critical in a number of different areas related to a multi-factorial concussion assessment.
At a minimum, the concussion assessment should include:
- Concussion history
- Personal and family medical history
- Mental health screen
- Symptom inventory / interview
- Computerized neurocognitive assessment
- Motor control, balance, and vestibular ocular assessments
- Physical cervical exam
- Patient-reported outcomes
The goal of the concussion assessment is to make decisions about treatment, referrals, or return to play, so it’s important to use tools that are sensitive and objective to detect impairments.
Treatment and Management
Athletic trainers are heavily involved in concussion treatment and management. The biggest advantage to athletic trainers’ involvement in concussion treatment is that they are easily accessible to patients and usually can see them daily if needed.
“Athletic trainers see their athletes on a daily basis and know them best. Athletic trainers are the best equipped and have the best training in assessment and management of concussions.” - Secondary School AT (From a survey of athletic trainers)
Clinical Profiles
Athletic trainers may use the information gathered during the clinical interview, symptom inventory, and objective assessments to determine a concussion phenotype / subtype / clinical profile to the patient and use it to direct treatment before starting any return to activity progression for work / school / sport.
There are 5 concussion phenotypes / subtypes / clinical profiles:
- Cognitive / Fatigue
- Symptoms: Difficulty concentrating, overall fatigue, decreased energy levels
- Treatment: Reduce cognitive and physical demands, regulate sleep, stress, diet, and mild exercise (1 short walk per day)
- Ocular-Motor
- Symptoms: Localized / frontal-based headaches, fatigue, distractibility, difficulty with vision, pressure behind eyes, trouble focusing
- Treatment: Consult with neuro-optometrist and vestibular therapist, vision therapy rehab with a specialist
- Headache / Migraine
- Symptoms: Moderate to severe headache with nausea and photosensitivity or phonosensitivity, often exaggerated by physical activity or stress
- Treatment: Pharmacologic intervention
- Vestibular
- Symptoms: Dizziness, fogginess, nausea, anxiety, overstimulation by complex environments, brought on by rapid head or body movements
- Treatment: Vestibular rehab
- Anxiety / Mood
- Symptoms: Overall increase in anxiety, perhaps with sleep disturbance and vestibular issues
- Treatment: Treat vestibular issues, begin physical exertion protocols, regulate sleep
There are also 2 concussion-associated conditions that can be associated with any of the subtypes:
- Sleep disturbance
- Cervical strain
Early Subsymptom Threshold Exercise
We know that patients benefit from an initial period of rest for no longer than 24-48 hours. After which, they benefit from early sub-symptom threshold exercise. Athletic trainers are well-positioned to administer sub-symptom threshold exercise and monitor patients during concussion recovery.
Multiple studies support the benefits of early aerobic exercise. Results have found that:
- Early aerobic exercise is effective in reducing symptoms and is safe to initiate following 48 hours of rest (Langevin, et al).
- Aerobic exercise was favorable in both acute and prolonged recovery cases to decrease symptoms and shorten recovery time (Powell, et al).
- Subsymptom threshold exercise beginning within two weeks of the injury had the largest effect sizes. All physical activity was found to be beneficial to recovery (Carter, et al.)
- Early aerobic exercise has shown promising results and does not appear to increase the risk of prolonged recovery (Del Rossi, et al).
Early exercise intervention has both physical and psychological benefits.
Physical benefits:
- Maintain fitness
- Physiological benefits of exercise
- Rehabilitation of affected systems
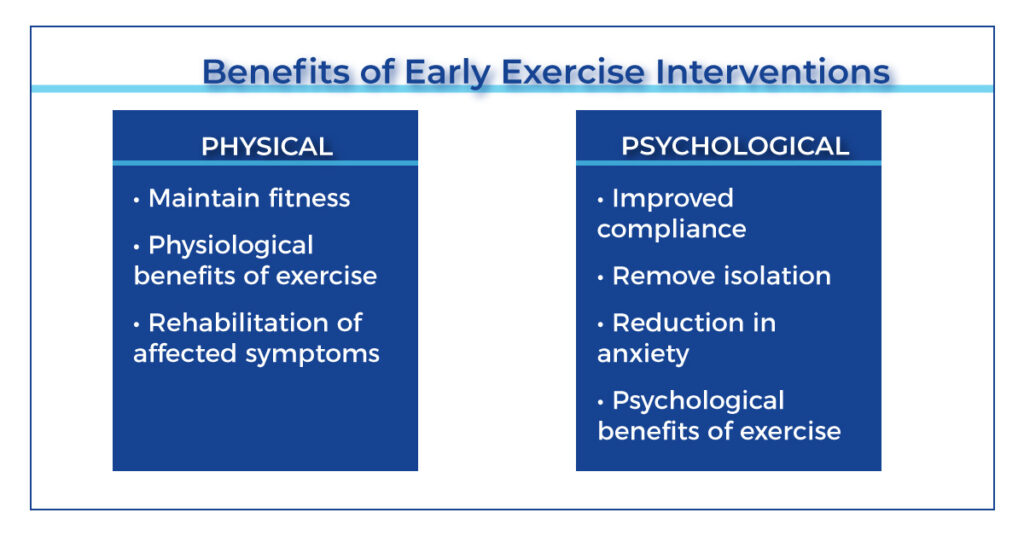
Psychological benefits:
- Improved compliance
- Remove isolation
- Reduction in anxiety
- Psychological benefits of exercise
Academic Accommodations
We know there are numerous benefits to getting students back into the classroom. However, patients may not be ready to return at full capacity, in which case, academic adjustments are provided. In order to facilitate academic adjustments athletic trainers should be aware of the academic supports available, laws and policies regarding academics, the roles of other members on the concussion care team, and best practices regarding managing concussions.
Academic adjustments can be categorized in three tiers.
Tier 1: Universal Level
Temporary academic adjustments that should ebb and flow as the patient needs. Teachers should feel empowered to liberally provide these academic adjustments to patients based on the information they receive from the athletic trainer or school nurse that gives them insight into the symptoms the patient is having.
Tier 2: Targeted Level
Formal academic adjustments often in the form of a 504 plan. The athletic trainer might be a part of the 504 committee that helps develop these, or they might be providing information to that committee to help support this.
Tier 3: Intensive Level
Permanent academic modifications. Concussion patients rarely end up in level 3 tier.
Exercise Testing
Exercise testing is another area where athletic trainers can have an important role.
There are a number of formal assessment including:
- Buffalo Concussion Treadmill / Bike Test
- Calgary Stationary Cycle Test
- Military Exertion Tests
- Gapski-Goodman Test
- Dynamic Exertion Test
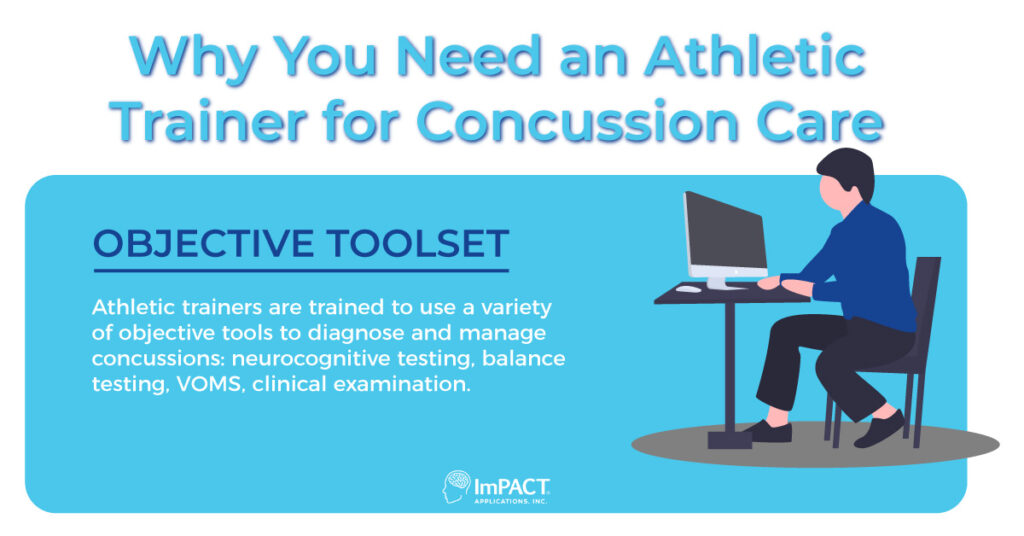
Concussion Testing
Athletic trainers can evaluate and manage concussions by using a variety of objective tools. Here are some of the assessments they may use:
Return to Activity
Athletic trainers have a critical role in return to activity and getting students back into school with the use of academic supports for returning to a full academic workload.
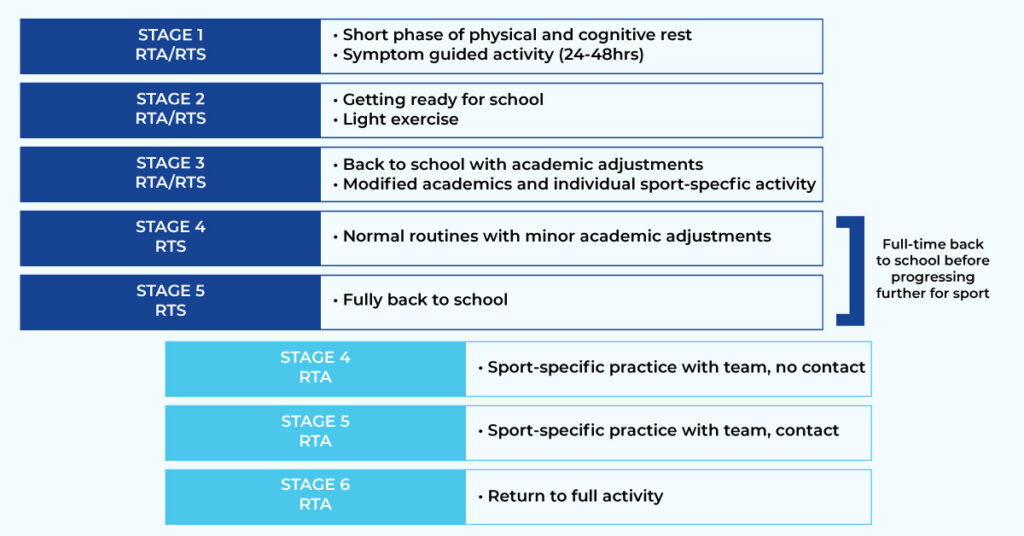
Return to Learn / Play
Research supports a 6-stage combined return to learn and return to play progression.
Return to Work
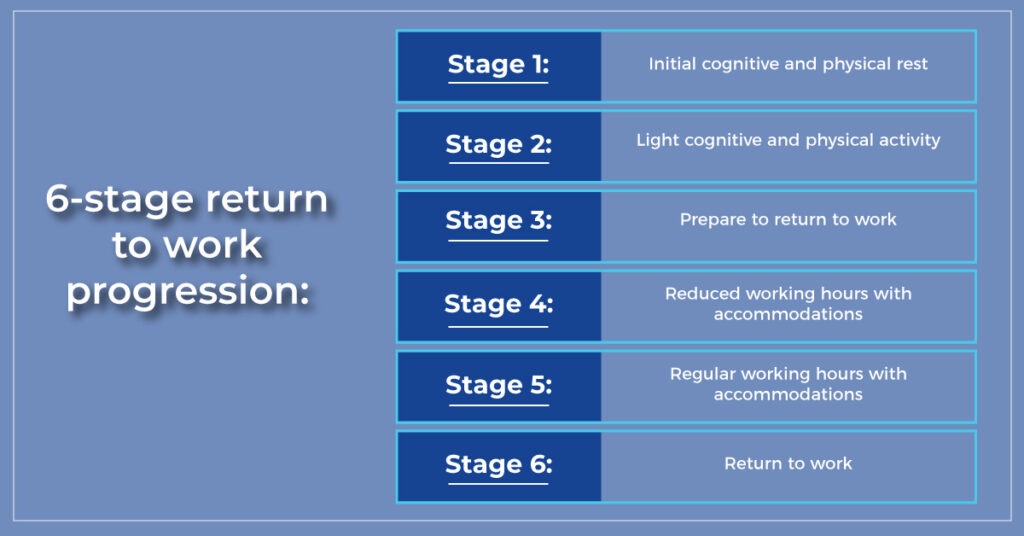
The athletic trainer may also be involved in return to work, working with the rest of the multidisciplinary team as well as the employer. Similar to academic accommodations, the patient may require workplace accommodations and adjustments based on their impairments to allow them to successfully return to work.
6-stage return to work progression:
Stage 1: Initial cognitive and physical rest
Stage 2: Light cognitive and physical activity
Stage 3: Prepare to return to work
Stage 4: Reduced working hours with accommodations
Stage 5: Regular working hours with accommodations
Stage 6: Return to work
Return to Driving
The athletic trainer can also be involved in counseling patients on return to driving. We know that post-concussion, patients have deficits in oculomotor control, visual processing, and reaction time. However, 44% of athletic trainers reported not providing any recommendations on return to driving.
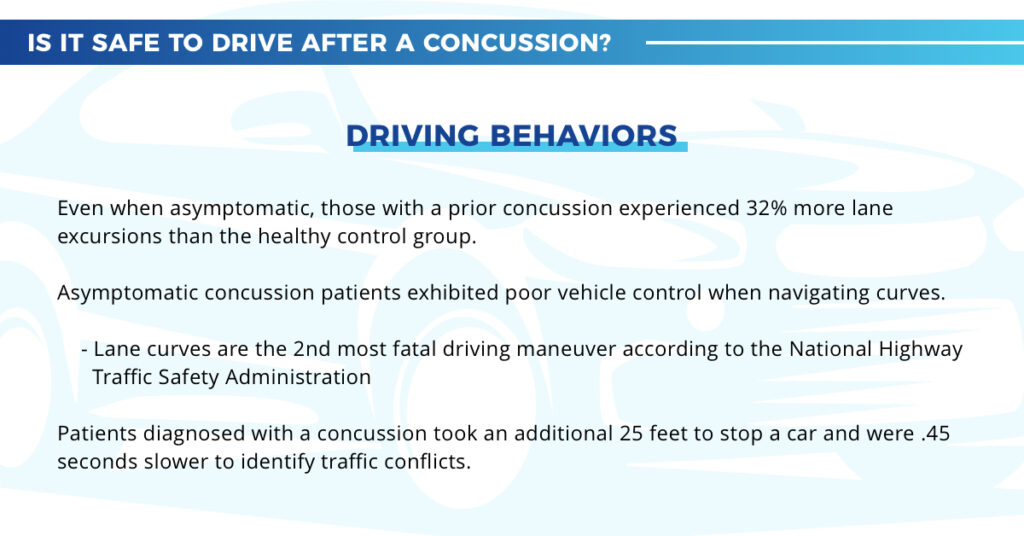
The athletic trainer should look at symptom assessments and cognitive impairments to help support their return to driving recommendations. ImPACT clinical reports include an objective measure of reaction time, which can be used as an indicator that the patient may not be ready to return to driving if they have impairments in this area.
Continued Care
Athletic trainers can play a role in concussion prevention, which can be broken into 3 categories.
Primary Prevention: protection from concussion happening in the first place. Takes place pre-season.
- Rule changes
- Behavioral modification
- Protective equipment
- Prevention interventions
Secondary Prevention: Limited long-term disability and preventing re-injury. Takes place post-injury.
- Legislation
- Education
- Identification and management
- Anticipatory guidance
Tertiary Prevention: Aims to soften the impact of an ongoing illness or injury that has lasting effects. The goal is to improve quality of life and mitigate persisting symptoms.
- Active treatments
Interprofessional Collaboration
Athletic trainers are critical members of the concussion care team. In the secondary school setting, the athletic trainer is usually the point person or case manager. In a survey of high school principals, over 50% agreed that the point person should be the athletic trainer.
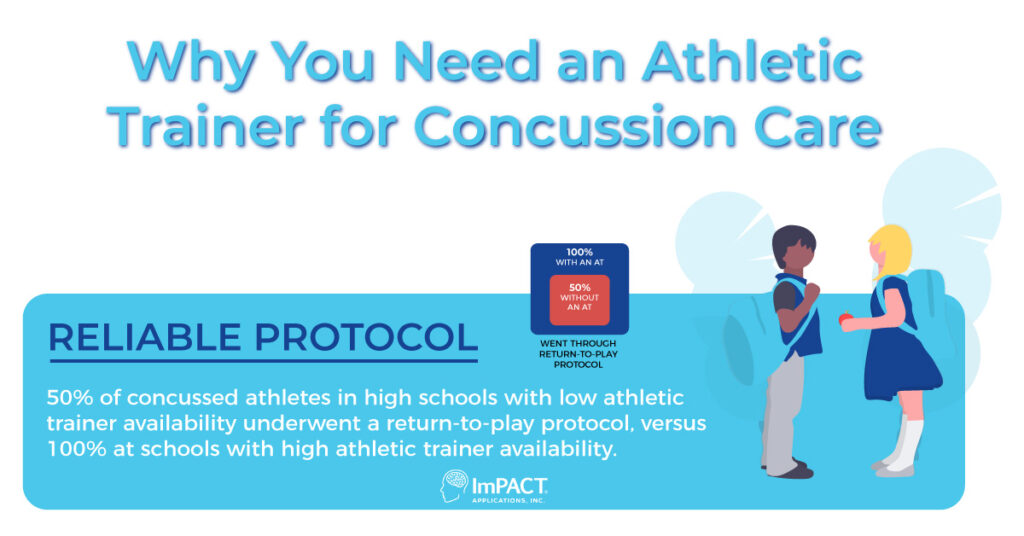
Advocating for a Greater Role in Concussion Care in Your Organization
Schools that have athletic trainers are seeing improvements in how they handle concussions. At the high school level, 50% of concussed athletes with low athletic trainer availability underwent a return-to-play protocol compared to 100% at schools with high athletic trainer availability. Schools with higher AT availability were also more likely to diagnose concussions and follow evidence-based guidelines.
There are a number of ways athletic trainers can advocate for themselves as important members of the concussion care team at any organization.
- Elevate your own practice.
- Educate parents, coaches, and administrators about what your scope of practice is and what you’re capable of doing.
- Integrate yourself with school administrators.
- Collaborate with the concussion management team and understand what each individual brings to the table.
- Articulate your knowledge, skills, and roles to patients, parents, community providers, and other concussion management team members.
Finding an Athletic Trainer for Your Organization
50% of schools currently have athletic training coverage. If your school or youth sports organization does not, you're leaving a large number of athletes and students at risk.

Search our directory of ImPACT Trained Athletic Trainers to find a local concussion specialist who can share more about the importance of their role.