Return to Learn / Work After a Concussion
Based on a presentation given by Karen McAvoy, PsyD, School and Clinical Psychologist. Concepts in the guide are credited to GetSchooledOnConcussions.com.
All 50 states have Return to Play legislation in place. Most concussion laws contain three action steps:
- Education: Educate various stakeholders about concussions - stakeholders will vary by state; usually includes - coaches, athletes, and parents - occasionally but rarely includes educators.
- Removal from play: An athlete with a suspected concussion should be removed from play immediately. (A sideline tool, like ImPACT Quick Test, can be used to help support removal from activity decisions.)
- Clearance for return to play: An athlete can only return to play after at least 24 hours and with permission from a qualified healthcare provider; qualified healthcare providers will vary by state. (A neurocognitive assessment tool, like ImPACT, can be used to help support return to activity decisions.)
Despite widespread Return to Play legislation, few states have language in their concussion laws requiring schools to establish a Return to Learn concussion protocol.
In 2020, the Delphi Consensus for Return to Learn was published. This established a consensus on 13 essential elements of Return to Learn from 15 national organizations.
Within the consensus statements there are six overarching themes:
The consensus statements for Return to Learn may also be applied for Return to Work in the adult population. Download this quick reference guide for Return to Work.
1
Return to School is not synonymous with Return to Learn.
Return to School: The process of the student physically walking back into a school setting. The decision to send a child to school on any given day is directed by the parent often with input from the healthcare provider and is dependent upon the student’s ability to manage symptoms well enough to be physically and cognitively present in the classroom setting to listen and learn (REAPconcussion.com©).
Return to Learn: The process by which educators help students with concussion maximize learning while minimizing symptom flare-ups. A successful Return to Learn plan is directed by educators who have knowledge and skill in differentiated instruction to meet the needs of all students regardless of medical, psychological, learning, behavioral, or social conditions (REAPconcussion.com©).
Consensus Statement #1: Students recovering from a concussion, but not all, often need an initial period of relatively greater cognitive and physical rest, the timing and specific nature of which will vary from student to student.
Consensus Statement #2: An estimated 70% of students recover from a concussion in 28 days with a gradual reduction of symptoms. This supports a gradual return to social and cognitive activity at home and school over the first four weeks of recovery. The speed of re-introduction will vary and must be individualized.
Consensus Statement #3: Numerous positive social and emotional benefits are gained by being at school, even during recovery from a concussion. Unless contraindicated by a serious medical complication, a student with a concussion should return to school/learn even before symptoms are 100% resolved, provided the student can manage fluctuating symptoms, and the school concussion management team has received education and resources to support the student in the educational setting.
There needs to be an initial period of cognitive rest followed by a gradual re-entry back into what patients were doing pre-concussion. We know from research that extended periods of rest can be detrimental and counterproductive to patients’ concussion recovery (Thomas, 2015). The 2013 American Academy of Pediatrics suggests that students should return to school when symptoms are tolerable, short-lived, and amenable to rest. This is usually after about 24-48 hours of complete cognitive and physical rest.
There are several ways to return a student back to school and each comes with its challenges. A couple common ones include:
- A graduated step-wise back to school process. This can be very difficult for schools because they typically don’t have the staff to be able to assess daily whether or not a student is tolerating 2 hours of cognitive activity every day and to know when to move them onto the next step.
- A red, orange, yellow, green process. This process is also difficult if schools are waiting for or requiring medical providers to help assess whether or not students can move to the next step. Since medical clinics are not seeing the patients every day, and some students never see a medical provider at all throughout their recovery, this is going to fall on school personnel which is very labor intensive.
It’s a common misconception that having school work sent home rather than going into the classroom setting is easier on the student with a concussion. Actually, it is less cognitively taxing for students to be physically in the classroom, listening passively and learning, rather than staying home teaching themselves content from a textbook and completing in-class and homework all on their own.
The work equivalent would be trying to work from home rather than going into an office setting. Compared to the school setting, return to work can be much more nuanced.
Some considerations for work from home vs. work in an office setting include:
- Can the job be done remotely?
- Can the patient be in the back of the office instead of the front of the office?
- Does the job have “light duty”? What is the pay?
The first big barrier to Return to Learn and Return to Work is students/employees must first Return to School/Return to the Work Setting (i.e., physically walk back into the classroom/work setting) before teachers and employers can even know where to begin to consider academic/work adjustments/accommodations.
2
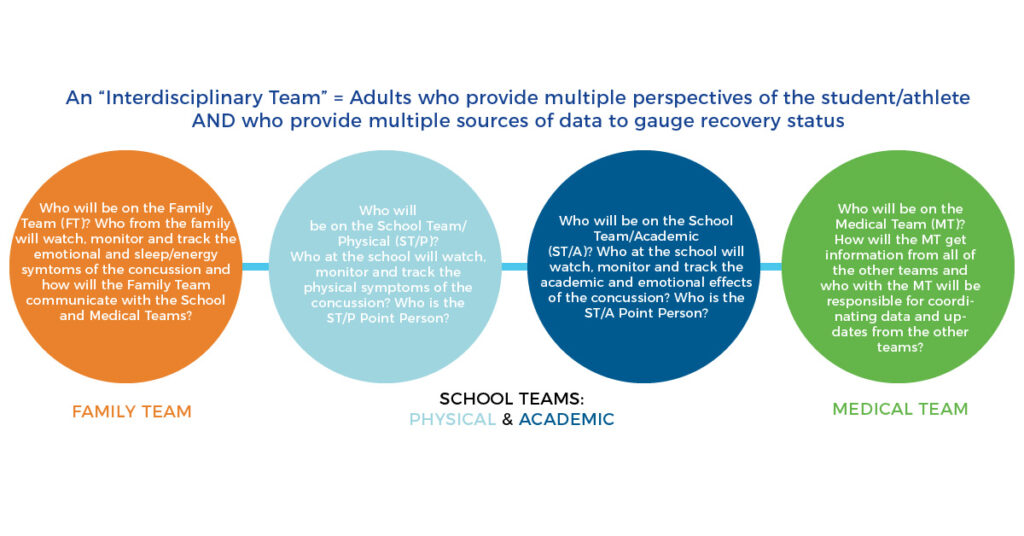
Consensus Statement #4: A concussion management team should include representatives from school academic school physical/health services, medical, and family/student domains who work collaboratively to develop and adjust an individualized Return to Learn plan.
Consensus Statement #5: A family is advised to seek out medical evaluation, specifically, a timely medical evaluation, treatment, and clearance for each concussion (regardless of the age of the student or the mechanism of injury).
An interdisciplinary team approach is critical for successful Return to Learn / Work and for concussion treatment and recovery as a whole. The interdisciplinary team should consist of the Family Team, School Teams (both Physical and Academic), and the Medical Team (REAPconcussion.com©).
Each team is working together to support students throughout recovery but may not all be doing the same treatment/management at the same time. Teams are passing the baton to one another as recovery progresses. This requires a lot of communication and respect for each other's different roles on the concussion management team.
3
Consensus Statement #7: Progress monitoring should include symptom monitoring no less than one time per week.
ImPACT Post-Concussion Symptom Scale can be used to monitor symptoms. Symptoms should be evaluated weekly to ensure patients are moving in the right direction.
Consensus Statement #8: Progress monitoring should include academic monitoring no less than one time per week.
Academic monitoring collects teacher feedback on how the student is doing and whether they’re back to pre-concussion learning levels. In the adult setting, this would be employer feedback on whether the employee is back to pre-concussion work and cognitive levels.
ImPACT can be used to assess cognitive levels and monitor progress. The objective data shows where the patient is cognitively at the start of their rehab and over time shows where they have progressed to / what areas they may be stalling in.
4
Consensus Statement #9: Schools have existing educational safeguards to support all students who struggle academically, medically, psychologically, and socially at school. Concussion can be included and managed using the existing educational safeguards.
Consensus Statement #10: Schools should provide increasing tiers of academic support for the students with concussions that do not resolve in a typical timeframe.
Consensus Statement #11: Schools may apply their existing tiers of support for students with concussion and need not delay or postpone academic supports while awaiting community health care input if medical input is not timely or available.
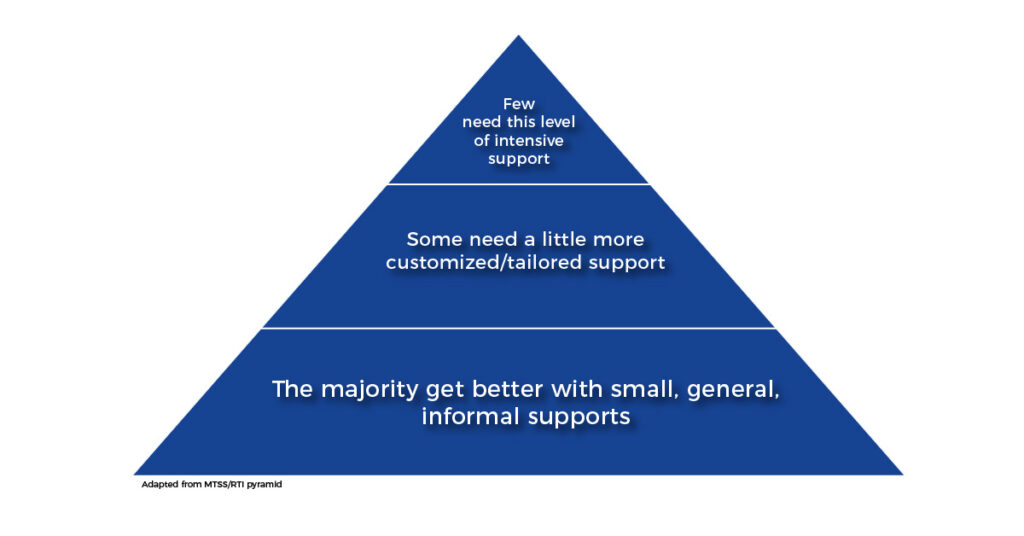
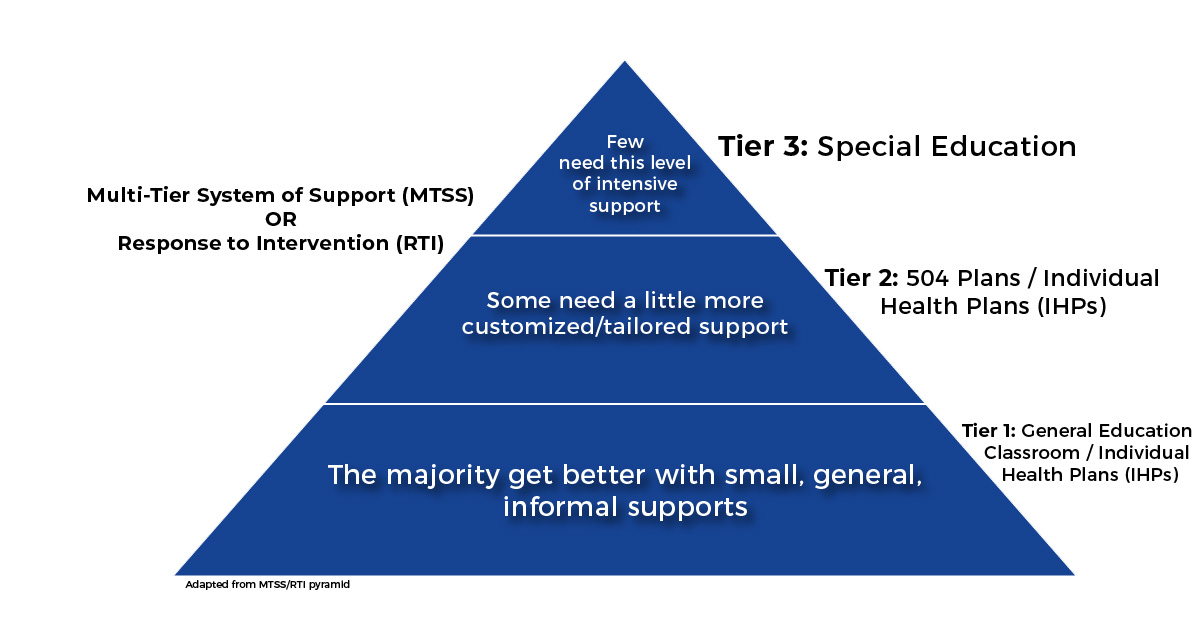
Schools have an existing educational model that allows educators to support all students who struggle at school - whether that be from psychological, medical, social, or behavioral reasons - there is an ascending level of support that is provided and students move through the different levels until their needs are met. This is an independent educational process that does not require medical input. This model, much like a public health model, outlines that the majority of students get better with small, informal, general support. A smaller portion of students will require a more tailored approach. And a very small number of students will need intensive support.
In the educational world, this is called the Multi-Tier System of Support (MTSS) or Response to Intervention (RTI).
Tier 1: General Education
Tier 2: 504 Plans / Individualized Health Plans (IHPs)
Tier 3: Special Education
MTSS or RTI is based on a few key concepts:
- Early screening and intervention
- Prevention - avoid bigger problems down the road
- Allowing time for interventions and data-driven decision making
- Ascending tiers will provide whatever level of support students need to succeed
Federal guidelines use MTSS or RTI for reading, learning, behavioral, social, medical, and psychological issues that impact students’ ability to learn. Concussions fit into an MTSS or RTI model. The problem is that educators have not taken ownership for Return to Learn after concussions. So out of necessity, many Return to Learn guidelines come from healthcare (medical and athletic) providers who are telling educators what to do to support students with concussion in schools. In an ideal situation, each team would own their own unique and vital part in concussion recovery and educators need to own Return to Learn.
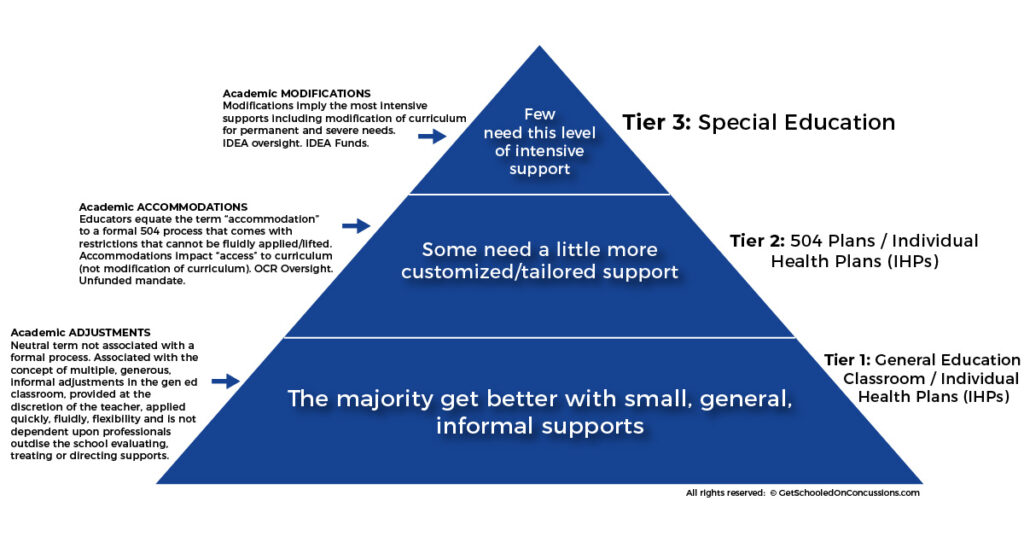
When we apply MTSS to concussion:
Tier 1: Academic "adjustments”
- Informal classroom supports that can be given and removed quickly at the discretion of the general education teacher
- Informal Individualized Healthcare Plans (IHP) may be initiated at Tier 1 or Tier 2
- Support happens over days to weeks
Tier 2: Academic “accommodations”
- Formal supports that require a 504 plan
- Support might take weeks or months
Tier 3: Academic modifications
- Allows for modification of the curriculum, specialized programming, instruction or placement - also known as special education
- Supports students months to years after their injury
Approximately 80-90% of students’ needs will be met in Tier 1 with simple academic “adjustments” that can be managed by Tier 1 educators (classroom teachers). However, students are often being jumped to Tier 2 because:
- It is difficult to reach thousands of classroom teachers to properly train and empower them to give immediate and flexible academic “adjustments” within the first 4 weeks post-concussion.
- There is more access to Tier 2 Related Service Providers (school nurses, counselors, school mental health professionals, administrators) because there are fewer of them to train and they can gather more easily for trainings. Tier 2 providers usually get involved with concussions at/after week 4. This is problematic because waiting until weeks 4-6 to get Tier 2 providers involved in RTL means schools have missed the “window of opportunity” to have classroom teachers support students in their classrooms through weeks 1-4.
To fix this problem, general education teachers need to be educated and empowered to provide academic “adjustments” immediately, flexibly, nimbly at Tier 1.
Educators at Tier 1 and Tier 2 need to “own” they are the experts in Return to Learn (post-concussion, post-illness, injury, trauma) post any medical/psychological diagnoses.
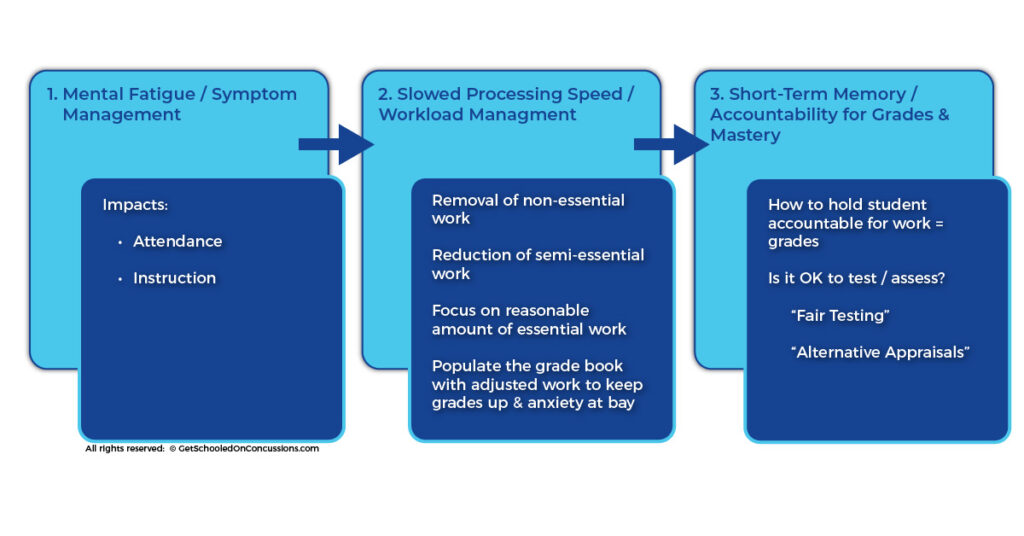
When educating teachers, GetSchooledOnConcussions.com suggests: focus on mental fatigue, slowed processing speed, and short-term memory, in that order. These impacts of the concussion translate directly into areas that teachers already know how to manage.
- Mental Fatigue → Symptom Management
- Energy management in order to attend school and hear instruction
- Slowed Processing Speed → Workload Management
- Removal of non-essential work
- Reduction of semi-essential work
- A reasonable amount of essential work for the individual student
- Short-Term Memory → Accountability for Grade and Mastery
- How to hold student accountable for work / grades
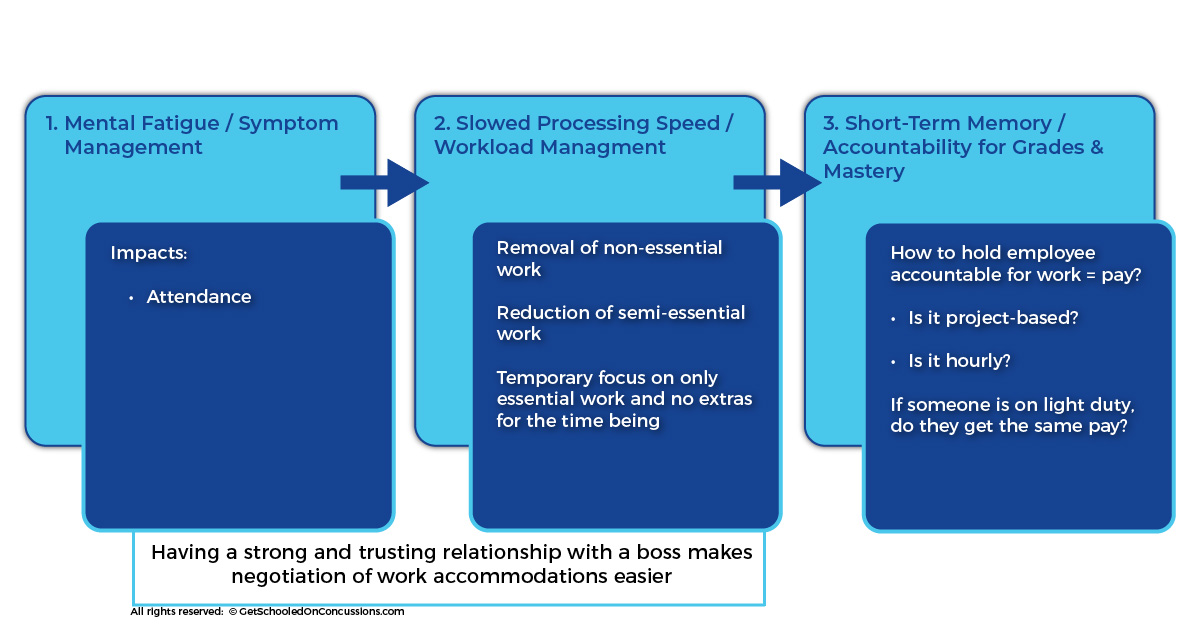
For adult patients, the same framework can be applied for Return to Work and work adjustments.
- Mental Fatigue → Symptom Management
- Energy management in order to attend work and complete tasks
- Slowed Processing Speed → Workload Management
- Removal of non-essential work
- Reduction of semi-essential work
- What is a reasonable amount of essential work for this employee? How best to support the concussed employee without having work fall on co-workers?
- Short-Term Memory → Accountability for Productivity
- How to hold employee accountable for work / pay
Having a strong and trusting relationship with an employer makes negotiation of work adjustments/accommodations easier. Unlike Return to Learn, there is the added consideration of pay for adult patients. It’s important to consider how they will be compensated (e.g. is it project based or hourly? Does light duty get the same pay?). There is also the added component that work settings often schedule based upon anticipated coverage per shift. Lightening the load for 1 employee, due to concussion, may inflict hardship on other employees.
Mental Fatigue / Symptom Management
Mental fatigue translates into symptoms and symptoms translate into whether or not you can attend school / work. Patients with concussion are working with “an outdated phone battery” or a “smaller gas tank” and need to learn to manage their energy so that they can manage their symptoms. To do so, they may need to take frequent breaks throughout the day. To state again the importance of first a Return to School/Work, /work supports cannot happen if students/patients are not first physically back in the classroom or the work setting.
Slowed Processing Speed / Workload Management
Once a student is back in school/work, then the teacher / employer can provide adjustments like removal of non-essential work, reduction of semi-essential work, and only focusing on a few clear expectations.
Short-Term Memory / Accountability for Grades and Mastery / Productivity
To test mastery or productivity, teachers/employers should consider alternative methods to testing such as:
- Oral presentation
- Video presentation
- Group work
If a teacher feels a test is necessary, they should make adjustments that may include:
- Open book
- Multiple choice
- Extended time
- No more than 1 test per day
These strategies are all within the teacher’s/employer’s purview and do not require medical approval.
The rule of thumb for testing at schools is to consider foregoing testing in the first 1-2 weeks post-concussion, then consider attempting some adapted assessments as recovery progresses into week 3 and beyond.
For adults returning to work, they need to discuss directly with their boss how much time they need to be working, how they will be evaluated, and what is fair pay for their adjusted work schedule and role.
Consensus Statement #6: Adjustments written into the Return to Learn plan are best overseen and directed by school professionals with dedicated expertise and knowledge of educational law, policy, and curriculum, guiding a collaborative Return to Learn process among the members of the concussion management team.
Return to Learn should be School/Work-Based and School/Work-Directed. Recommendations from healthcare providers are suggestions not mandates. Recommendations from professionals outside school or work settings are often unrealistic and tie the hands of the educator/employer. Absolute recommendations tend to lead to over- or under-compliance. Instead, healthcare providers should explain the medical condition and let schools / work come up with interventions appropriate to their own settings. Teachers / Employers should be allowed to apply or lift supports as needed and move students / employees up through higher levels of support if they are not responsive to lower levels of interventions.
Here are some examples of how healthcare providers should communicate Return to Learn / Work recommendations to schools / work.
If the patient is experiencing slowed processing speed…
INSTEAD of saying “exempt student from in-class work and homework” or “exempt employee from being on the retail floor”...
EXPLAIN that learning and thinking is less efficient after a concussion.
SUGGEST teachers consider removal of non-essential work, reduction of semi-essential work, flexible due dates, and alternative ways to keep up with learning and show mastery.
SUGGEST employers consider temporary light duty and working in a less public-facing role or location (e.g. working in the back instead of at the cashier).
If the patient is experiencing convergence insufficiency…
INSTEAD of saying “don’t allow the student / employee to use the computer”...
EXPLAIN that cognitive insufficiency is the inability for the eyes to focus near to far. This often manifests as eye strain and headaches.
SUGGEST teachers consider preferential seating, audio books, giving the student a copy of the notes, keeping screen time to a minimum and allow for breaks, giving the option for oral presentations instead of testing for the first few weeks.
SUGGEST employers consider doing things on paper instead of a computer, allowing for self-paced work, not introducing new learning during recovery, adjusting computer font and size.
5
Consensus Statement #12: Data from a neuropsychological evaluation is not required, but can be helpful and should be considered and may be incorporated into a Return to Learn plan if available.
The consensus statement says that conventional neuropsychological testing, while not required, can be helpful. However, there are many barriers to neuropsychological testing:
- Usually cannot get into neuropsychological testing within 4 weeks
- May provoke symptoms if done too early into recovery
- There are limited neuropsychologists to administer the testing
- Expensive and time consuming
- Not easily replicable
ImPACT is a great alternative for a number of reasons:
- Can be administered by any trained healthcare provider (not limited to neuropsychologists)
- Administered in just 20 minutes
- Not too symptom provoking
- Cost effective
6
Consensus Statement #13: Existing educational safeguards exist for students. They are prompt, flexible, and systematic for all concussed student athletes and non-athletes with academic needs. Return to Learn can be robust, widespread, systematized, and sustainable if embedded into existing educational frameworks.
This consensus statement supports Return to Learn that fits into the existing educational framework that was outlined throughout this guide.