Creating Tailored Concussion Rehab Plans
Addressing concussion care in non-athletes in the post-COVID world
Based on a presentation given by Nathan Diffenaugh, MSPT, DPT, Rehabilitation Manager at Lehigh Valley Health Network, at the 2021 Concussion Care Virtual Conference.
How to Create Tailored Concussion Rehab Plans
for Non-Athletes
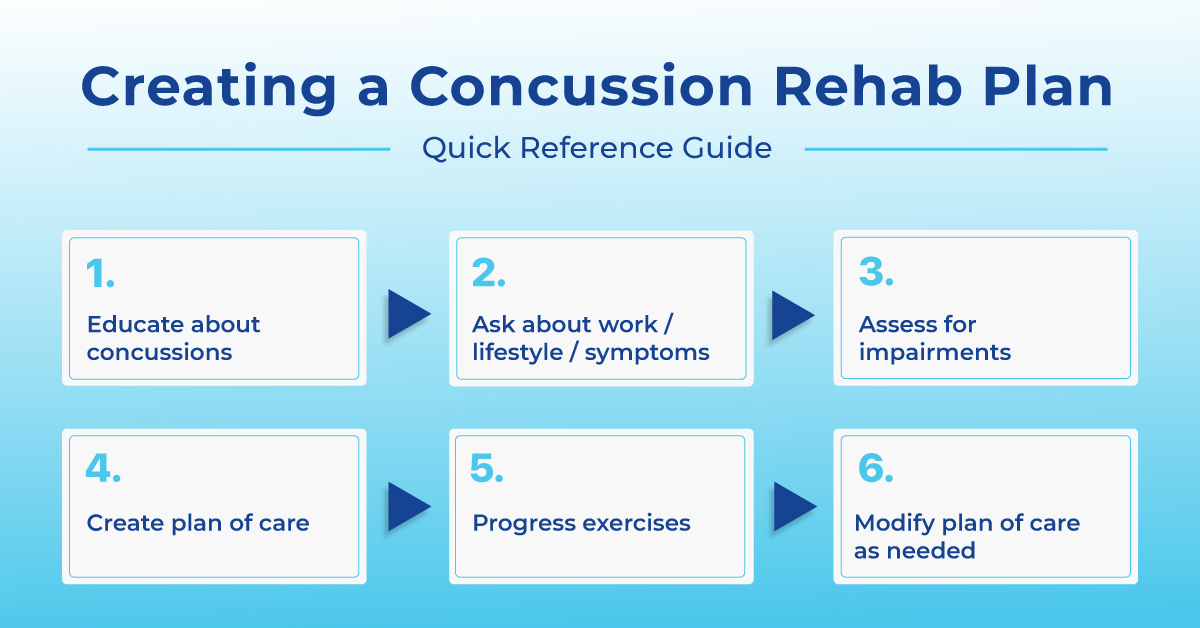
Step #1: Educate patients and set goals for therapy.
Step #2: Ask patients about their recreational activities.
Step #3: Ask patients about their job duties.
Step #4: Assess the patient.
Step #5: Create a plan of care that addresses specific deficits.
Step #6: Progress the exercises.
Step #7: Return to work and modify the plan of care.
Table of Contents
Concussions are talked about in sports all the time but are much less commonly talked about when it comes to non-athletes. The reality is, concussions happen among all ages and all types of people.
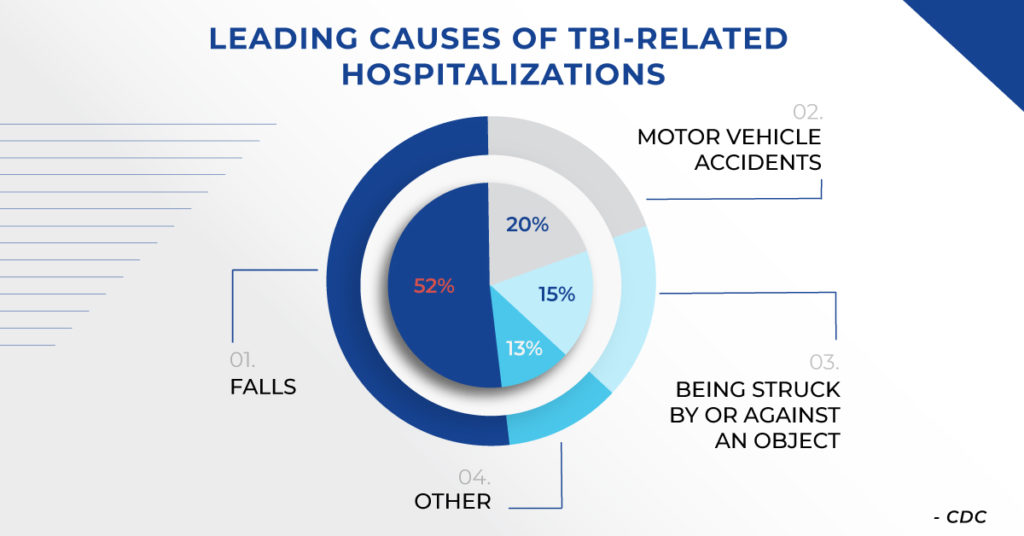
In fact, the leading cause of concussions is actually falls. According to the CDC, in 2014 almost half of all TBIs were from falls, across all ages. In patients over the age of 65, 4 out of 5 TBIs were from falls.
Before creating a treatment plan, make sure patients understand why they were referred to therapy and what you are going to do to help their ongoing symptoms. Ask patients about the symptoms they’re experiencing and what they hope to accomplish in therapy. These goals might be specific, such as getting back to work or being able to read. Or they may be more vague such as to stop getting dizzy or stop having headaches.
Start by asking patients what they want to be able to do after therapy to determine what functional areas need to be addressed in your plan of care to get them where they need to be.
When athletes come in with a concussion, the goal is to get them back into the game. We ask what sport they play and what their position is.
For example, if we have a patient who plays soccer as a goalie, we know we’ll have to work on hands, coordination, and do some conditioning. This may be a little different for a patient who plays baseball who needs to be able to run and see the ball.
For the non-athlete, the goal is to get them back into the “game of life”. Ask patients what they do for recreation and use that as a starting point for creating your plan of care.
For example, someone that spends a lot of time reading or playing video games may need to address some oculo-motor aspects that can be affected by a concussion. On the other hand, you may have a patient who likes to do more social activities like go to parties, attend concerts, or travel. This person will be in busier environments and may have things that challenge their balance that you’ll need to address. Another example is a parent that coaches their 6 year old son’s baseball team. This person will need to be able to run, keep their eyes moving, show the kids how to hit the ball, move positions, etc.
Desk jobs
What’s their job / industry?
How many screens do they use?
Do they work in a team or do they work independently?
Do they have to interact with clients / customers?
Do they work from home? If not, are they in their own office, a cubicle, or open space?
Physical labor jobs
Do they have to go up and down ladders?
Do they have to move heavy objects? Approximately how much weight? How often?
Are they in a warehouse? Do they have to operate or work around heavy machinery?
Stay-at-home jobs
Do they take care of children / grandchildren? How old are they?
What are their household duties?
What is their home environment? Do they live in a single-story or multi-story home?
Students
What are they studying?
Are their classes virtual, in-person, or hybrid?
Do they typically study at home or in a public place?
Are they involved in group projects or is their work independent?
Common Work-Related Complaints After a Concussion
Intolerance for using a computer
Typically, someone complaining about intolerance for using the computer is having some issues with saccades. They may also be having issues tolerating light.
Intolerance for busy environments
Someone complaining about intolerance for busy environments may be having issues with smooth pursuits, visual tracking, or changing distance between near and far objects.
Intolerance for physical labor
Intolerance for physical labor may be caused by motion, physical exertion, or change in position. Ask questions about what bothers them specifically to determine what is causing their symptoms.
If they experience symptoms when they are in a moving car or riding on the forklift, they may have some VOR and visual tracking issues. If patients experience symptoms after a lot of physical exertion, take a look at what they can tolerate and give them drills related to their job duties for them to practice. If patients experience symptoms when they move their head, they may have BPPV in addition to their concussion that needs to be addressed.
Inability to focus on tasks
Clarify whether they are having trouble paying attention to the task or if they are having trouble visually focusing. If the problem is attention to the task, take a closer look at memory and cognition. If the problem is visually focusing, take a closer look at oculomotor function.
Motion sickness
Determine if it is a peripheral or central problem. Assess for peripheral dysfunction and treat BPPV if it is noted.
Have they had issues with this before?
Do the symptoms last only a few seconds?
Do the symptoms only come if they bend over?
Have they had any changes in their hearing?
Have they had any ringing in the ears? If so, one ear or both?
When it comes to assessment, you’re going to use a similar approach for non-athletes as you would for athletes. You’re going to ask about symptoms, determine limitations, and find a solution. Your basic toolkit of exercises does not change.
At a minimum you should assess:
- Balance
- Cognitive function (ImPACT)
- Smooth / visual pursuits
- Near / Far
- Saccades
- VOR
Create a rehab plan that addresses the deficits identified during the assessment. Explain what each exercise is addressing and how it will help patients return to their job or daily activities. For example, VOR exercises will help with returning to driving, saccade exercises will help with reading, and balance exercises will help prevent another fall.
Combine tasks
You may have patients work on VOR while walking or have them read something and try to remember it then walking over to another area and answering questions about what they just read.
Work-specific tasks
Make exercises relevant to their job duties or the activities they want to return to. For example, if they have a desk job you might have them enter data in a spreadsheet or pretend to write emails on various topics. If their job involves lifting items, you might place dumbbells around the clinic and the patients will have to walk around and pick them up and move them. For students, you might have them bring in homework so you can watch them work on it and see what’s triggering symptoms.
Review their home exercise program (HEP)
When patients return to work, instruct the patient to lower the frequency of the home exercises they’re doing and advise on when to do them. For example, you may have been having the patient do the HEP 3-5 times a day when they weren’t in school or work. Now, you may suggest they go to school / work, come home and rest for a bit, and do the HEP once in the afternoon and once in the evening as tolerated, then back to 3-5 times a day on the weekends.
Have them keep a symptom log
Give the patient a symptom log that includes activity, symptoms, duration (either duration of the activity or duration of the symptoms). Whenever they get symptoms, instruct them to record the activity they were doing, what symptoms they experienced, and either the duration of the activity they were doing or how long the symptoms lasted.
Review the symptom log at your next visit and ask targeted questions about what they were doing when they experienced the symptoms. For example, if they started feeling dizzy in math class when they were taking notes because they had to look back and forth between their notepad and the whiteboard, this tells you they may be having problems with near / far tasks.
Use information from the symptom log to modify the plan of care to address specific work / school triggers.
Importance of home exercise programs (HEPs)
Home exercise programs (HEPs) are especially important when patients are not coming into the clinic, or coming in less frequently. With virtual visits, you must educate patients even more on how to monitor their symptoms including tracking what their symptoms are, how long they’re lasting, and if they’re improving over time. Additionally, educate them on how to progress the home program if they start to feel better before your next appointment. This may include standing instead of sitting, having the TV in the background instead of a blank wall, increasing the speed at which they’re doing the exercise, or standing on a pillow instead of a hard surface.
Safety is key
There are exercises you may have patients do in the clinic that you don’t feel comfortable with them completing at home without you there. For exercises you do have them carry out at home, you may advise they hold onto the countertop or have someone with them when working on balance exercises to prevent a fall.
Shift to an educational model
Virtual visits require you to go into more of an educational model where you give the patient the knowledge to care for themselves. Instead of watching them do the exercises, you are teaching them the exercises and how to progress them and having them show you that they understand.
Red flags / need for in-person visit
Not all patients are a good fit for virtual visits. Some red flags that would warrant an in-person visit include:
- Fall risk
- Inability to treat positional vertigo
- Signs / symptoms inconsistent with the injury
Assessment
When conducting an assessment via telemedicine, utilize testing that can be patient-led such as the Motion Sensitivity Quotient (MSQ) and Vestibular/Ocular Motor Screening (VOMS). Have the patient complete the exercise themselves and report their symptoms.
Have the patient complete ImPACT remotely via telemedicine. It will generate the same clinical report as when the patient completes it in-person which gives you valuable insight into their cognitive status and how they’re progressing.
Start “basic”: Safety is an important consideration for virtual visits and it may not be safe to have the patient do some exercises right away. We may have them start sitting or wait to do balance exercises if we’re worried about them falling.
Send educational material ahead of time: Email the patient before their appointment with the exercises you plan to do.
Use what’s available: You won’t have access to the same equipment for virtual visits that you do in the clinic. Some common household items that can be incorporated are sticky notes, pencil, magazine, textbooks, pillows / blankets, TV, YouTube.
Consider a hybrid approach: Use clinic days to re-evaluate and progress the program. Use virtual days to touch base and issue variations to the program.
Limitations to virtual visits:
- Intolerance for screen time
- Patient safety
- Limited equipment
- Difficult to visually assess the patient