Creating a Profitable Concussion Management Program
Learn how Premier Health implemented their clinic-based concussion management program to get consistently reimbursed, increase patient acquisition, and maximize downstream revenue.
Based on a presentation given by Shad Bernard, Central Region Manager of Sports Medicine at Premier Health, at the 2022 Concussion Care Virtual Conference.
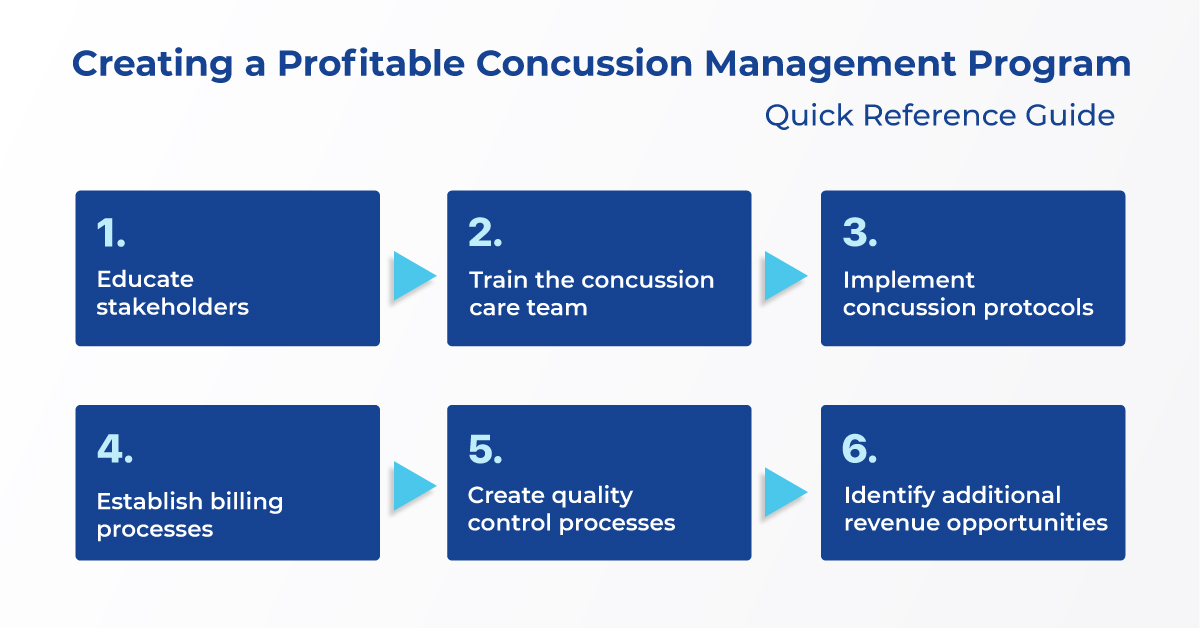
How to Create a Profitable Concussion Management Program
1. Ask, “Who are the key stakeholders?”
2. Get training for the multidisciplinary concussion care team
3. Implement concussion protocols at the clinical and school levels
4. Establish billing best practices and processes
5. Create quality control processes
6. Identify other revenue opportunities outside of sports
Located in Dayton, Ohio, Premier Health consists of 5 large hospitals, including 2 sports performance centers, and 1606 hospital beds. Premier Health partners with 40 high schools across 9 counties, 4 universities, 30 police and fire departments, and 4 YMCA and recreational facilities, making them the largest sports medicine outreach provider in Southwest Ohio.
As a result of the Zurich guidelines introduced in 2008 and concussion care becoming an emerging issue in high school sports, Premier Health knew they needed to re-evaluate how they were managing concussions in order to meet new best practices. In 2012, Premier Health conducted an extensive review of their current concussion management protocol and how that was being implemented in the clinical setting and within their partner schools.
In the school setting, they found that out of their 40 partner high schools, only 17 were using ImPACT for concussion management and they were only baseline testing “high-risk” sports such as football, wrestling, and soccer. These schools were also handling post-injury testing themselves, rather than referring to a physician, which meant there were no standardized testing standards across the organization.
In the clinical setting, they found that only 1 physician was utilizing ImPACT in their office for post-concussion care. They also found that they did not have any billing established with the office for neuropsychological testing by computer.
In the end, they accepted that they had a broken system to care for and manage concussions in both the clinical and school settings.
Knowing they had to improve their concussion management protocols to meet the new standards of concussion management, the physician and sports medicine leadership teams created a business plan outlining how they would generate downstream revenue while establishing best practice protocols for concussion management. This plan was presented to the hospital board, who granted them $300,000 to establish new concussion management protocols and implement them within their clinical setting in order to provide the highest level of care to all of their athletes and community members across the Dayton, Ohio area.
In order to implement new procedures, it’s important to get buy-in from all stakeholders. Identify individuals or departments that your new procedures will impact and educate them on the benefit of what you’re doing.
Executive leadership: Create and implement new protocols.
Physicians: Adapt to new billing procedures and workflows.
Physician office managers: Adjust workflows and scheduling for the physician.
Supply chain: Help meet technology and equipment requirements for ImPACT.
Legal: Help bring partner organizations under one ImPACT Applications agreement.
Physical Therapists / Occupational Therapists: Help generate downstream revenue by offering additional services.
Athletic trainers: Implement concussion protocols including ImPACT baseline testing in partner organizations.
School partners: Become familiar with new concussion protocols and ImPACT.
Billing: Examine billing codes and processes to maximize reimbursement.
IT: Establish reliable connectivity in the clinical setting.
Decision support: Provide reports on billing code usage.
ImPACT Applications: Provide concussion testing and help with implementation.
Step #2: Get training for the multidisciplinary concussion care team.
One of the first things Premier Health did was have their concussion care multidisciplinary team members complete an ImPACT Applications’ credential program to ensure they all have the same baseline level knowledge about how to manage concussions and utilize ImPACT. In the first two years, 21 physicians completed the Credentialed ImPACT Consultant (CIC) program, 74 athletic trainers completed the ImPACT Trained Athletic Trainer (ITAT) program, and physical therapists completed the ImPACT Trained Physical Therapist (ITPT) program. These credential programs are now part of their onboarding process for new hires. They also cover the cost of the annual continuing education course which is a requirement to maintain each credential.
Step #3: Implement concussion protocols at the clinical and school levels.
Premier Health provides athletic training services to their partner schools including implementing the concussion protocol and administering ImPACT baseline testing. They cover the cost of ImPACT for their partner schools to baseline test ALL athletes, no matter their sport. In light of the pandemic, Premier Health athletic trainers switched to at-home baseline testing in 2020 and have continued to utilize this home testing model to streamline administration.
They also decided that ImPACT post-injury testing would only be administered in the clinical setting, rather than being carried out at the school level by the athletic trainers like it had been in the past. This would help ensure standardized administration and help with billing and reimbursement.
If a head injury is suspected, the athlete is first evaluated by a Premier Health athletic trainer at that school who completes the Premier Health Concussion Packet which includes an extensive evaluation form. If the athlete would like to see a Premier Health physician, they can choose from a list of their CICs who will conduct ImPACT post-injury testing and create a tailored treatment plan. The athletic trainer will send their evaluation to the physician prior to the patient visit so they don’t have to rely solely on the athlete’s recollection of events. Premier Health athletic trainers work closely with the physicians to communicate with the schools regarding education plans and academic accommodations.
Step #4 Establish billing best practices and processes
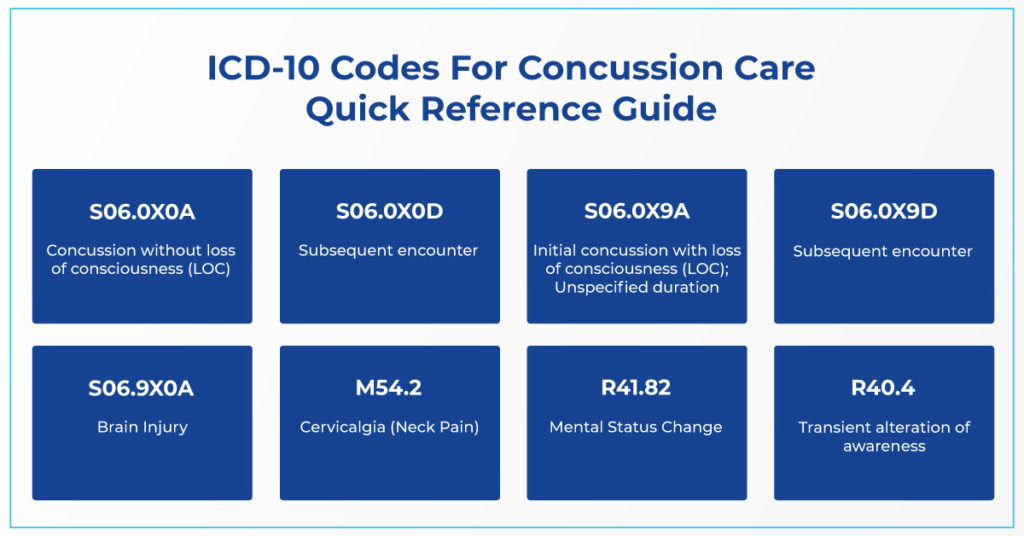
The most commonly used ICD-10 diagnosis codes for concussion care are:
S06.0X0A - Concussion without loss of consciousness (LOC)
S06.0X0D - Subsequent encounter
S06.0X9A - Initial concussion with loss of consciousness (LOC); Unspecified duration
S06.0X9D - Subsequent encounter
S06.9X0A - Brain Injury
M54.2 - Cervicalgia (Neck Pain)
R41.82 - Mental Status Change
R40.4 - Transient alteration of awareness
The two diagnosis codes most frequently used by Premier Health are S06.0X0A and S06.0X9A. It’s a good idea to err on the side of caution and use S06.0X0A unless you have specific documentation that shows LOC, in which case the use of S06.0X9A is warranted. Use S06.0X0D or S06.0X9D for subsequent encounters when the patient returns for post-concussion care after the initial visit.
Use M54.2, R41.82, or R40.4 when the patient displays any of these symptoms in addition to their concussion. Including modifiers adds additional value to the office visit.
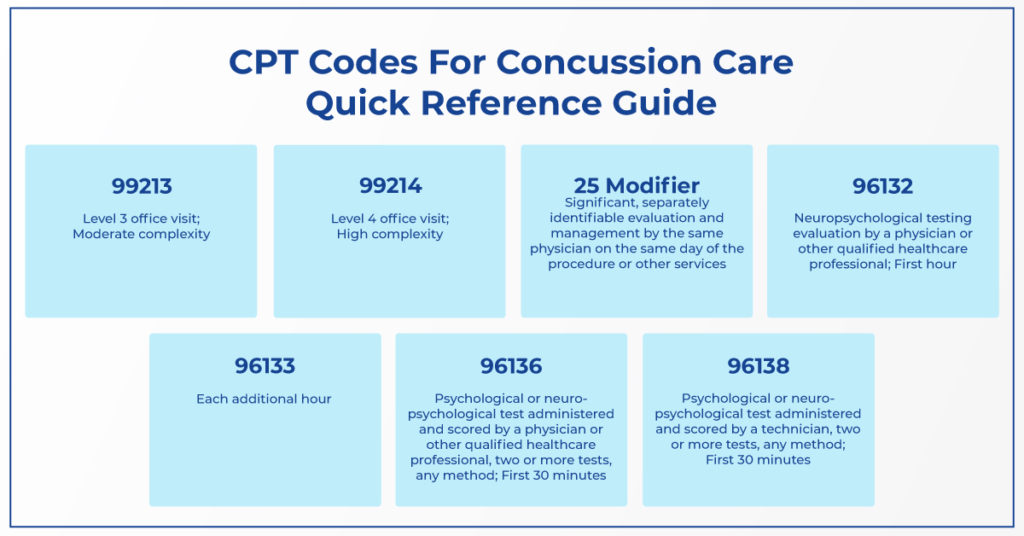
The most commonly used CPT codes for concussion care are:
99213 - Level 3 office visit; Moderate complexity
99214 - Level 4 office visit; High complexity
25 Modifier - significant, separately identifiable evaluation and management by the same physician on the same day of the procedure or other services
96132 - Neuropsychological testing evaluation by a physician or other qualified healthcare professional; First hour
96133 - Each additional hour
96136 - Psychological or neuropsychological test administered and scored by a physician or other qualified healthcare professional, two or more tests, any method; First 30 minutes
96138 - Psychological or neuropsychological test administered and scored by a technician, two or more tests, any method; First 30 minutes
Reimbursement for Telemedicine Visits:
Telemedicine became a vital part of Premier Health’s concussion care when they needed to increase access to patient care during the COVID-19 pandemic. Since then, they’ve taken advantage of the ability to distribute unique ImPACT testing links in the Customer Center for patients to complete remotely. They’ve had a highly successful rate of individuals completing ImPACT remotely using their unique testing link and have been consistently reimbursed for virtual visits at the same rate as in-person visits.
Scenario #1:
The medical assistant (MA) brings the patient into the exam room, the physician stops in and has a conversion with the patient and decides whether or not they can cognitively handle taking an ImPACT post-injury test. They deem the patient capable and the MA administers the test. The physician comes back into the room and finishes their examination and goes over ImPACT results; 1 hour.
In this scenario, you’d bill 96132 for neuropsychological testing evaluation by a physician or other qualified healthcare professional for the first hour.
Scenario #2:
The Physician’s Assistant or Nurse Practitioner does the initial assessment and administers ImPACT, without the patient seeing the physician; 30 minutes.
In this scenario, you’d bill 96136 for scoring by a physician or other qualified healthcare professional for the first 30 minutes.
Scenario #3:
The medical assistant administers ImPACT before the patient sees the physician.
In this scenario, you’d bill 96138 for administration by a technician.
When to use the 25 Modifier:
For any of the scenarios, you can use the 25 Modifier in addition to the CPT code when your patient talks about other symptoms in addition to their concussion such as neck pain or confusion.
Step #5: Create quality control processes
Establish relationships with office billers
Within Premier Health’s network, physicians are broken down into two main groups: specialists and general family practice. It was important for them to talk to office billers to make sure they’re billing and coding consistently throughout the entire physician network.
Create consistency
Premier Health found that before establishing guidelines, all of their physicians were coding slightly differently. With the help of the Decision Support team, they identified the most frequently utilized codes and worked with their EMR provider to create smart phrases to ensure consistency in the language used by the physicians in their charting. Doing so has significantly decreased their number of declined charges and increased the amount of reimbursement from both private and commercial insurance carriers.
Conduct regular billing audits
Premier Health conducts quarterly audits with their physician office billers in which their Decision Support team will generate a report on each of the billing codes that shows for each physician, how many times that code was used and what the reimbursement rate was for each. They also review the billing codes they’re using on an annual basis, as they can change.
Conduct regular concussion protocol reviews
At Premier Health, all new physicians must complete the Credentialed ImPACT Consultant (CIC) program, which covers best practices in concussion management, how to interpret ImPACT clinical reports and use them to help create treatment plans, as well as billing and coding for concussion care. Additionally, Premier Health spends time making sure new physicians understand their specific billing and coding procedures including choosing a diagnosis code and the language to include along with it.
Step #6: Identify additional revenue streams
Urgent Care:
In many cases, urgent care is an untapped market for initial concussion care. Premier Health identified the need for concussion management outside of the normal clinical hours. They addressed this gap in care by expanding their concussion care services to their 9 urgent care locations, where patients could be seen after-hours and on weekends. By establishing concussion management in their urgent cares, they allowed patients to get earlier access to care and start the clock on their treatment and recovery process.
Their urgent cares act as a triage point to evaluate concussions and identify next steps in care. When a patient visits one of Premier Health’s urgent cares with a suspected concussion, a CIC-trained advanced practice provider will conduct the initial concussion evaluation including an ImPACT post-injury test. They will then refer the patient to a CIC-trained physician within the Premier Health system.
Since most urgent cares already perform annual physicals, Premier Health started offering ImPACT baseline testing as an add-on to any sports physical, allowing them to expand their reach beyond their partner schools. Additionally, ImPACT baseline testing is reimbursable when included as part of an annual physical.
Learn more about how to manage concussions in the urgent care setting.
Industrial Medicine:
Head injuries are the second leading time factor for individuals in worker’s compensation cases. Premier Health is talking to businesses about putting athletic trainers in the industrial medicine setting to care for their workers and provide baseline testing as part of their employee onboarding process.
Fire and Police Departments:
Similar to worker’s compensation, head injuries are the second leading time off factor for police officers and firefighters. Through Premier Health’s “Healthy Heroes” program, athletic trainers spend time at firehouses and police departments providing concussion care and incorporating ImPACT baseline testing into their onboarding process.
YMCA and Recreational Facilities:
98% of Premier Health’s patients are 13 years of age or older, and of the small percentage of youth patients, only 7% had completed a baseline test. Premier Health started providing ImPACT baseline tests to youth athletes in YMCA and recreational facilities to begin establishing relationships with them in hopes that they will come back to their clinic should they sustain a head injury.
Premier Health saw a successful commercial insurance reimbursement on 91% of claims and had a 7% increase in office visit revenue by utilizing multiple and consistent diagnosis codes.
They’ve had CPT codes 96132 and 96128 consistently be reimbursed at $152.50. Their average reimbursement for a specialist office is $107.72 per case, and their average reimbursement for a family practice office is $82.70 per case. This only includes reimbursement for neuropsychological testing done in the office via computer. This is additional revenue on top of their Level 3 or Level 4 25 modifier office visit charges. Premier Health has also seen their telemedicine visits being reimbursed at the same rates as in-person visits.